Prescription Tracking Service - NHS
Current hospital pharmacy systems relied heavily on manual tasks, creating operational backlogs and longer waiting times for patients, posing a potential health risk that the hospital needed to address. Recognising this gap, we focused on the most congested parts of the process as an opportunity to streamline workflows and reduce pharmacists’ cognitive load. To ensure efficiency and consistency during development, I established a comprehensive design system and component library. This foundation enabled the rapid creation of high-fidelity, browser-native prototypes, accelerating development and delivering a smoother, more intuitive user experience.
Client
NHS
DELIVERABLES
Create an application that enables pharmacy staff to efficiently manage, track, and dispense prescriptions from receipt to completion.
Year
2023
Role
UX Designer
03 SOLUTIONS DISCOVERY
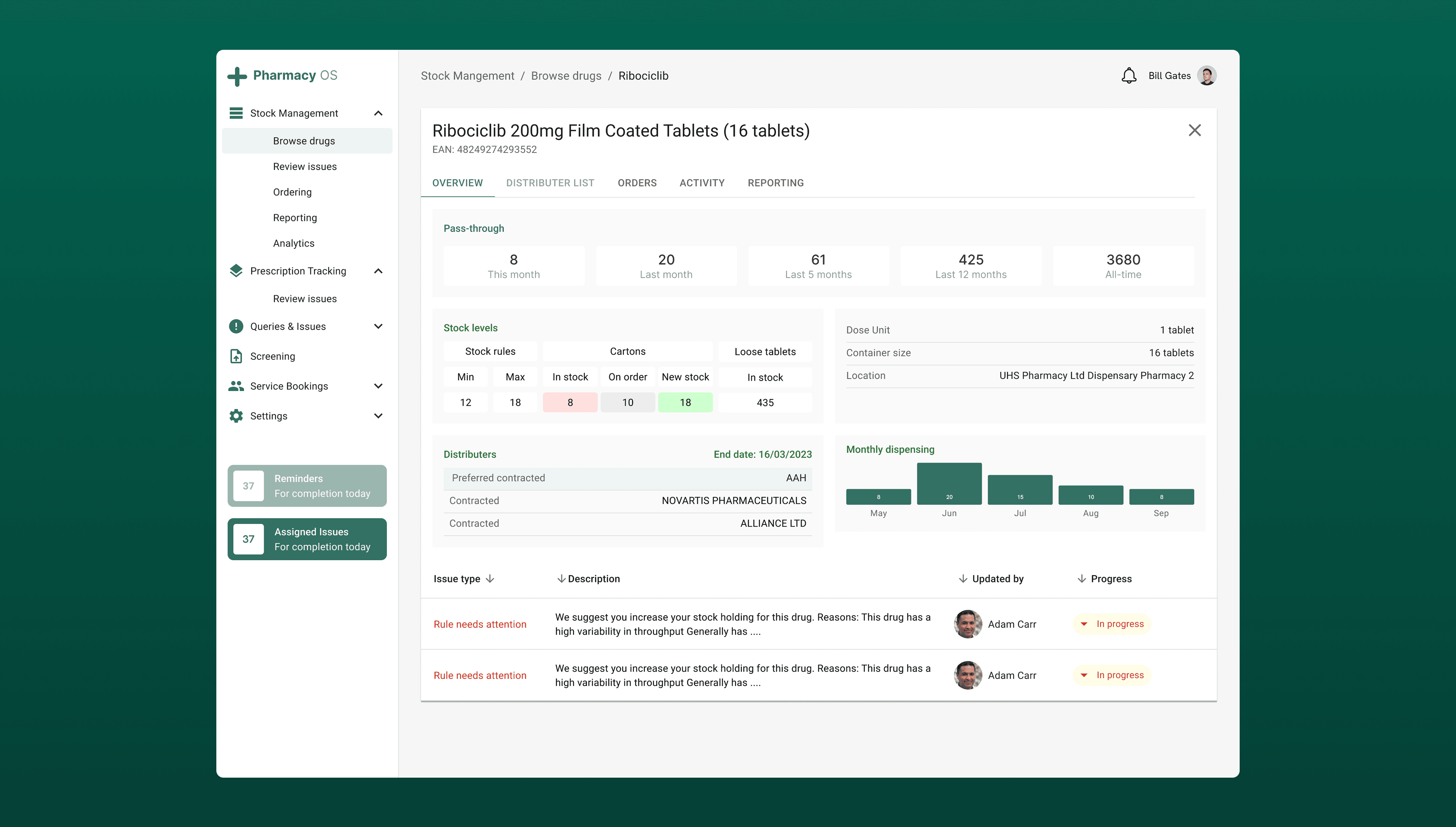
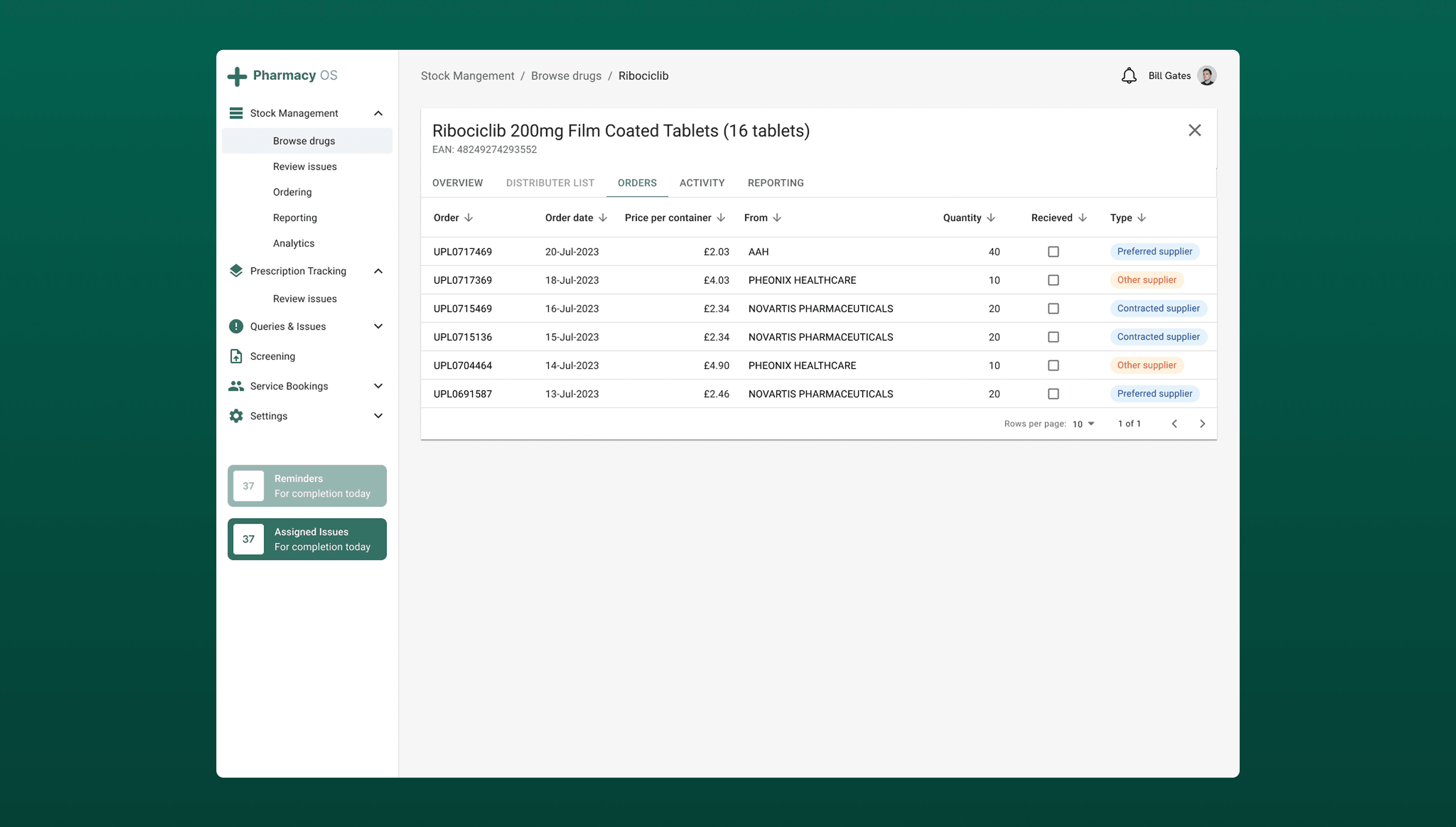
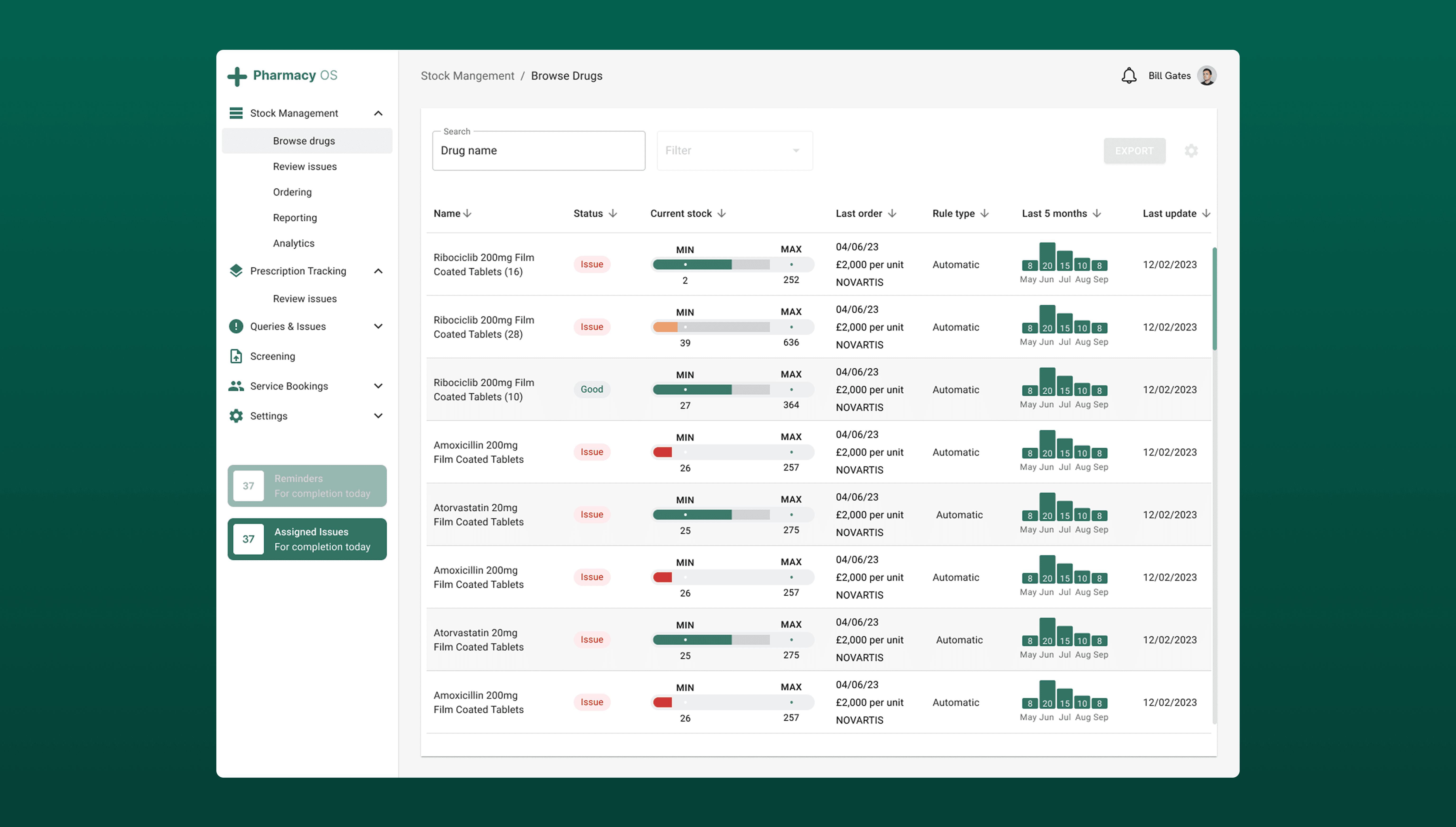
From our research, we found the systems used at the time were heavily reliant on manual processes, including printing and scanning prescriptions, handwritten annotations to adjust medication dosages and quantities, and the use of multiple systems to manage a single task.
I employed the RICE scoring method to prioritise which potential features to explore objectively across different areas such as potential impact, reach, effort required for each feature.
For the next 2 sprints we focused on:
Adding labelling guidance to streamline and automate prescription labelling and minimise room for errors.
Clear update progress to reduce number of queries related to timing of prescriptions.
Compulsory stock check entries to minimise the number of incorrect bookings being made on the system.
Add a tagging system so users are aware of which responsilbities are allocated for them to handle.
04 WHAT OUTCOMES ARE WE TRYING TO DRIVE
We developed key metrics to accurately measure how well the system performs and to guide data-driven improvements. These metrics reveal what’s working, highlight areas for optimisation, and help ensure we focus on meaningful outcomes. Key metrics are important for me for two main reasons
Goal-setting – Key metrics define clear targets and measure progress, ensuring efforts stay aligned with the right objectives rather than just activity.
Performance monitoring – They track performance over time, helping to spot trends and address potential issues early.
This is how I am sure that I am making informed decisions that align with company’s goals and objectives.
Outcome | How we'll measure it |
|---|---|
Labelling rules for prescriptions are adhered to and used | [Metric] # of users who have viewed the rules |
Clear understanding of responsibility within the team | [Metric] # of queries waiting after 48 hours |
Faster dispensing cycle – Less time spent answering timing questions means more time spent on actual dispensing. | [Metric] # Track the number of prescription-timing queries logged [Metric] # Percentage of prescriptions dispensed on or before estimated time |
05 SOLUTIONS & RESULTS
My approach focused on streamlining the prescribing process to deliver a smoother, more efficient platform for dispensing medication. After launch, prescription queries dropped by 35% thanks to clearer team responsibilities. Simple UX enhancements, such as a tagging system, enabled users to allocate enquiries and resolve tasks more quickly.
Usability testing confirmed these improvements: users reported that the new system was easier to use, analytics showed fewer clicks per task, and average prescription dispensing times fell from 11 minutes to just 6 minutes.
06 DID WE SOLVE OUR PROBLEM?
Yes. Our goal was to reduce delays and confusion in prescription dispensing and the results above demonstrated a direct solution to the original problem. From a business perspective, faster dispensing meant more prescriptions processed per day, reducing overtime costs and freeing pharmacists to focus on clinical care.
07 WHAT I WOULD DO DIFFERENTLY
Next time, I’d run an additional pilot with a live but low-risk prescription queue before full rollout. This would let us observe real-time bottlenecks (e.g., peak-hour handovers) that are harder to detect in moderated usability tests. I’d also set up automated dashboards (possibly in Power BI) from day one to continuously track dispensing times, tagging usage, and common error points, so we could act on data trends immediately rather than waiting for a post-launch review.